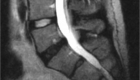
Disc herniation / Bulging disc
Bulging disc is one of the most common findings on spine imaging, MRI or CT scan. I am often asked if it is the cause of the neck or low back pain and whether it is dangerous and needs to be treated.
The short answer is: most often, NO. No treatment is required in most cases, but as just like with everything else, it depends.
The important point to remember: it is the symptoms that matter, not just findings on imaging.
Basic anatomy of a normal disc
Intervertebral disc is a sponge-like layer of tissue between two spine bones called vertebrae. In the mobile spine there are 25 vertebrae and 23 discs between them. The discs give the spine its flexibility and serve as shock absorbers.
There are two parts of the disc:
- Soft internal core called nucleus pulposus;
- Fibrous outside ring called annulus fibrosus.
Nucleus pulposus feels to touch like crabmeat or silly putty. It is what provides the bouncy properties to the disc. Annulus fibrosus is tougher. It surrounds the nucleus and prevents it from spreading out beyond its boundaries. You can think of a disc as a doughnut with filling.
The normal disc is flush with the nearby bones and does not protrude outside its boundaries.
What is a disc bulge?
If the outer layer, the annulus fibrosus, loses its strength, becomes thin or develops tears, the nucleus pulposus may escape its boundaries and push outwards. This is called a disc herniation or a bulge. Both terms may be used interchangeably. You may also find an abbreviation HNP (Herniated Nucleus Pulposus.)
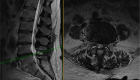
Different kinds of bulging discs
Even though any disc pushing outside its normal boundaries is considered herniated, there are several kinds of disc bulges presenting with different symptoms and treated differently.
I am not trying to make radiologists out of my patients, but since most people will read their radiology reports, let me give you a brief explanation on different types of bulges:
- Protrusion (also called prolapse): when the outside layer of the disc, the annulus fibrosus, is extending beyond the bone edges but annulus pulposus is not pushed outside of the annulus;
- Extrusion: when the soft nucleus pulposus is pushed outside of the annulus fibrosus;
- Sequester: when nucleus pulposus is not only pushed outside of the annulus but is also disconnected from it.
There may be other abnormalities of the disc without its fragment pushing outwards (not technically considered a bulge but you will find them in radiology reports):
- Hyperintensity zone: it is a tear in the annulus fibrosus;
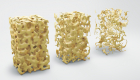
- Degenerative disc disease (DDD): when the disc looses it’s normal water content and turns black on MRI;
- Discal cyst: a fluid-filled bubble protruding from the disc.
Extrusion, sequester and discal cysts tend to respond better to surgery than protrusion, DDD and annular tears.
As always, I recommend that you talk to your spine specialist to understand what the imaging findings mean and whether they require anything more than just acknowledgment.
Symptoms of a bulging disc
I will need to repeat this several times: most bulging discs found on imaging do not cause any symptoms. Several scientific studies showed presence of disc bulges in most healthy people of different ages with no symptoms at all. As such, they are considered a normal part of aging.
Depending on the kind of disc abnormality and whether the bulge is pushing on the nerves, it may produce three kinds of symptoms:
- Axial back pain – this one does not respond to surgery well;
- Pinched nerve causing shooting pain into the leg, often called sciatica – surgery may help but there are other less invasive options to try first;
- Cauda equine syndrome – this requires immediate surgery.
If a herniation happens in the neck, this may cause:
- Arm pain called radiculopathy – surgery may help but is avoidable;
- Myelopathy if the bulge pushes on the spinal cord – this may require surgery.
So, let’s repeat this again: it is not enough to just obtain an MRI to decide what to do. You need to discuss findings with a spine specialist, who will correlate the imaging with your symptoms.
How do I know if the disc bulge is causing my pain?
There are several ways we can confirm or disprove that the bulge is the source of your symptoms:
- Clinical correlation: whether location of pain, numbness and weakness matches distribution of the pinched nerve;
- Electrodiagnostic studies (EMG/nerve conduction): an invasive study when needles are placed in the muscles of the arm or leg and nerve conductivity is tested. It may show abnormality in cases of compressed nerves.
- Diagnostic injections: if pain goes away after the affected nerve is injected, this confirms it is the source of pain.
The more the tests match your symptoms, the higher the chance that surgery may be effective.
When does a disc bulge require treatment?
As I mentioned before, disc bulges are very common on imaging of healthy people without any pain. As such, in most cases disc bulge does not require any treatment.
Even if there is pain extending into your arm or leg, in most people it will go away within eight to ten weeks.
More aggressive treatments may be required in the following cases:
- If the pain is not going away after a month or two;
- If there is progressive weakness or if you have red flags – symptoms suggesting that something dangerous may be going on.
Nonsurgical treatments
In cases when the bulged disc causes pain, there are several options to consider. If this is the first time you are having the problem, there is about 80% chance it will resolve by itself within one or two months.
A brief period of rest, local heat or cold, over the counter anti-inflammatory medications and Tylenol will improve pain in most people.
If pain does not go away after two-three weeks, physical therapy or chiropractic manipulation is the next step. Injections are reserved for the cases that don’t respond to any of the above treatments.
Surgery may be needed only in the minority of patients, who have pain despite the less aggressive treatments or when there are concerning findings like progressive weakness or changes in the bladder or bowel function.
When is surgery indicated?
Indications for surgery in the presence of disc bulges are very limited:
- Pain that is not going away with other, less invasive treatments.
- Progressive muscle weakness;
- Red flags (see below);
Red flags/emergency situations
As mentioned above, in some cases the bulge may produce severe pressure on the nerves causing the following symptoms:
- Difficulties with hand function, like tossing coins or buttoning a shirt;
- Progressive difficulties with balance;
- Weakness in the arms or legs;
- Inability to control bladder and/or bowel, rapid decline in sexual function;
- High fever and chills – this may indicate infection and not just a simple disc bulge.
If you have noticed any of these symptoms do not wait for them to go away, but discuss with your health provider as soon as possible. Stop letting spine pain control your life. Schedule your consultation with me today and take the first step towards lasting relief. Your journey to a pain-free life begins now. Click here to book your appointment.
What kinds of surgery are available?
Surgery typically involves removal of the bulged portion of the disc in order to “unpinch” the nerve. In very few patients fusion of the spine bones may be required, when there is an abnormal amount of motion between them.
Are there any dangers if bulging disc is left untreated?
No, unless there is pressure on the nerves, a bulging disc is not dangerous and does not require any treatments.
How do I find more information?
To find out what kind of treatment may be right for you, message us through the Contact Us form.