Degenerative disc disease (DDD)
Degenerative disc disease, frequently referred to as DDD, is a term that describes changes in the spinal disc occurring with age. Let us look at those changes, whether they may be the source of pain, and what treatments are available.
Anatomy of a normal intervertebral disc
Normal disc is a layer of elastic tissue lying between two spine bones called vertebra. The picture shows anatomy of a normal disc (also may be spelled as “disk” – both spellings are acceptable.)
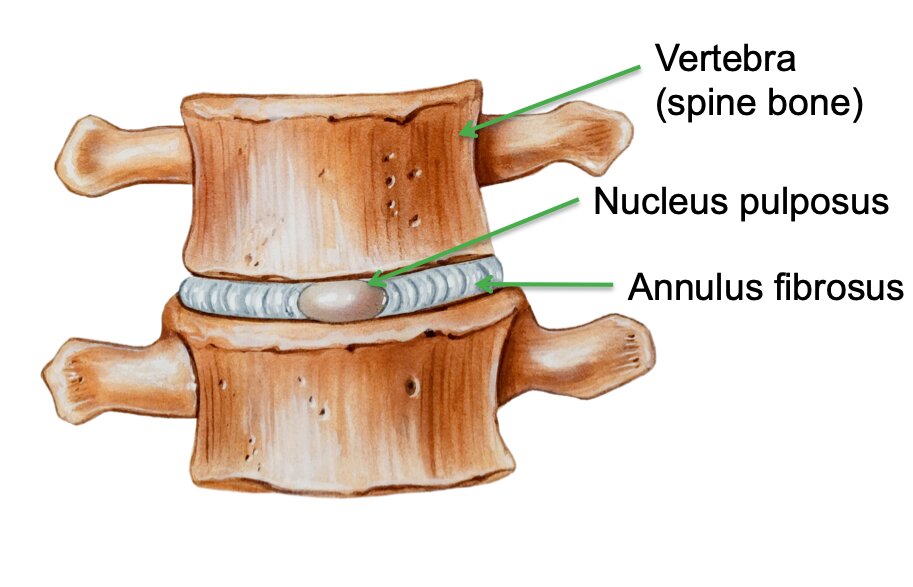
Figure 1 Schematic appearance of a normal intervertebral disc
The disc has two layers: the central part, called “nucleus pulposus”, acts primarily as a shock absorber. The nucleus contains high amount of water that provides its elastic properties.
The outer part of the disc, called “nucleus fibrosus”, surrounds the nucleus and prevents it from escaping the center of the disc and spreading towards the nearby structures.
You can think of the disc as a doughnut filled with jelly.
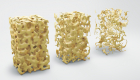
Development of DDD
Degeneration of the disc refers to its wear and tear. It starts with loss of water content leading to decreased elasticity of the disc. The annulus fibrosus becomes fragile and may develop cracks, through which nucleus pulposus (the core of the doughnut) may escape and compress the nearby nerves.
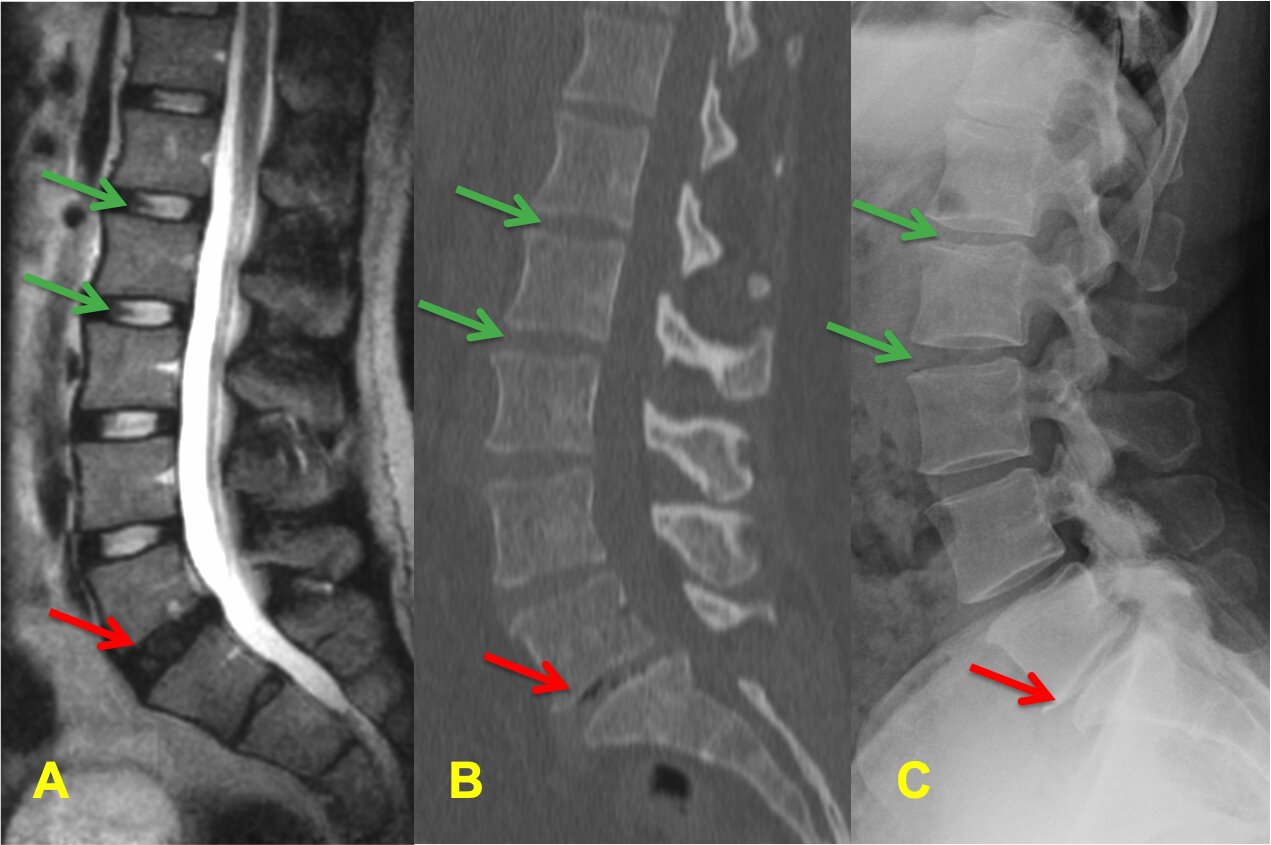
Figure 2 Side view of the same spine on MRI (A) CT-scan (B) and X-ray (C). Green arrows point at the normal discs. The red arrow point at a degenerated disc that appears dark and narrow.
The disc looses its height, which launches a cascade of changes in the nearby spine structures:
- Facet joints on the back side of the spine experience higher loading and develop arthritis causing instability between the bones and back pain
- Soft tissues lose tension, buckle up and may start pinching the nerves
- The body tries to stabilize the degenerated disc and develops bone spurs that in turn may compress the nerves
- Loss of disc height will follow and may lead to development of a disc bulge increasing pressure on the nerves
What are the symptoms of DDD?
In most people DDD will have no negative consequences. It is not a dangerous condition and is commonly found incidentally on imaging.
In the rare cases when symptoms are present, people complaint back pain and pain, numbness and tingling radiating in the legs. With severe pressure on the nerves, neurological symptoms may develop including leg weakness and changes in bowel and bladder function.
Pressure on the nerves may lead either to pain in the leg, radiculopathy (commonly known as sciatica) or neurogenic claudication (inability to walk distances due to nerve compression).
Where does the pain come from?
There are several structures in the spine that may produce pain: facet joints, muscles, soft tissues, pinched nerves, and the disc itself. Changes in the surrounding structures, like the facet joints, cause back pain most often.
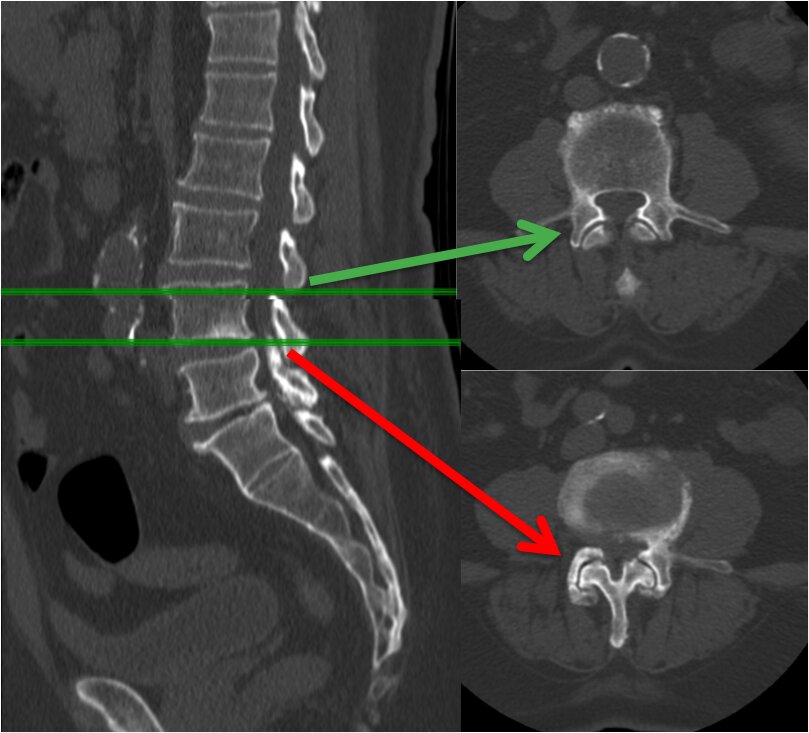
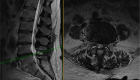
Figure 3 The right side of the images shows the cross-section of a CT-scan. You can see the facet joints located in the back of the spine. The green arrow points at a normal joint and the red arrow at a changed and degenerated joint that may be the source of pain.
How is DDD diagnosed?
There are three main imaging modalities we use for spine (Fig.2):
- X-rays
- CT (computed tomography)
- MRI (magnetic resonance imaging).
Each of them may show changes in the spine but from a different angle. X-ray and CT may show narrowing in the disc space, development of bone spurs and air inside the disc.
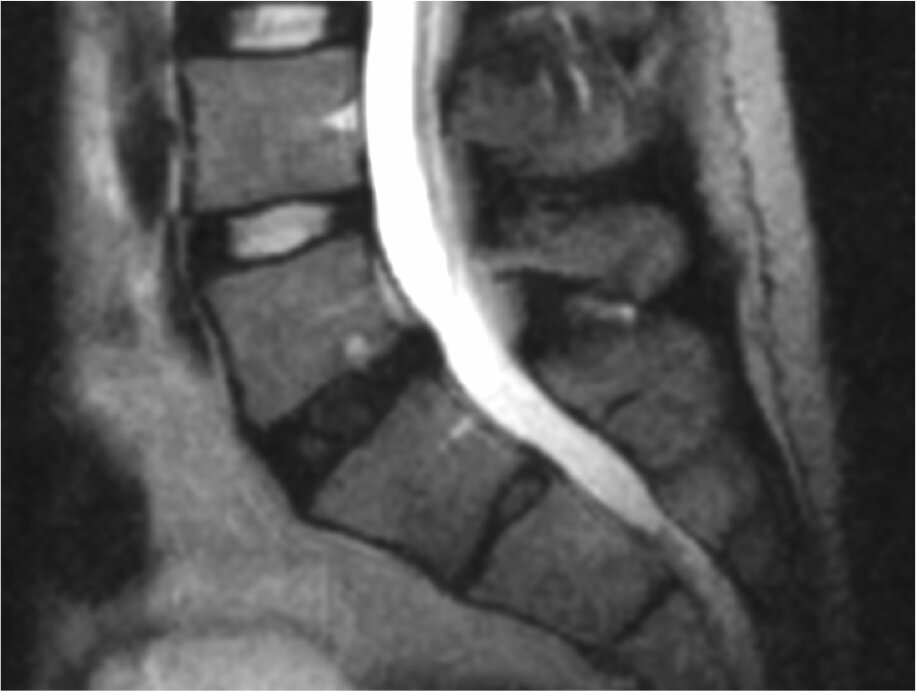
MRI is the most sensitive study and will show the early changes in the disc including early loss of water content (so-called “black disc”). MRI is the best study to visualize the soft tissues and see the amount of nerve compression.
Because MRI is very sensitive, it often shows changes not causing any symptoms. As such, it needs to be interpreted with great caution.
When is treatment needed for DDD? Will I need to have surgery?
Most cases of DDD are asymptomatic and won’t require any interventions. Treatments are considered only if symptoms are present. Otherwise, there are no dangers in ignoring it.
Surgery may be indicated in rare cases if the symptoms are resistant to less invasive options or if there is compression of the nerves resulting in progressive weakness.
Each patient’s situation is unique. To discuss your case and see what treatments are most appropriate for you, request an appointment for a face-to-face consultation.
Available treatments
Once degeneration of the disc has started, it cannot be reversed. Some new biological treatments are under investigation, including stem cell therapy, but the results are still not conclusive.
All currently available treatments are directed at the symptoms and not at reversal the disease itself.
Most people will not require surgery. Even if the symptoms are present, there are less invasive treatments that help in most cases:
- Self-care options:
- modification of activities
- over-the-counter medications like Ibuprofen, Naproxen and Tylenol
- Physical therapy and chiropractics
- Prescription medications
- Injections
How often do you see DDD?
Degenerative disc disease is seen on imaging in most people with age. Scientific studies estimate that roughly fifty percent of fifty-year-old, healthy and asymptomatic people will have degenerative changes on MRI. Based on this, unless you have symptoms, there is no need to obtain an MRI. Otherwise, this may lead to unnecessary treatments.
Why do some people develop disc degeneration and others don’t?
We don’t know the answer to this question. The two most likely players are genetics and environmental factors: obesity, smoking, and heavy physical labor.
Prevention of DDD
As of now, the best recommendations for keeping your spine healthy is to focus on a healthy lifestyle:
- stay physically active
- watch your weight (with the goal for Body Mass Index, BMI, below 35, and ideally below 25)
- do not smoke
- avoid excessive stress
Watch this video from North American Spine Society to learn about healthy habits for healthy spine.
If you have any additional questions, send us a message or request an appointment by filling out an online form.